Patient characteristics
A total of 249 patients underwent POP surgery during the study period, and 23 patients with primary vaginal vault POP after the previous hysterectomy were excluded. Of the 226 patients enrolled for primary POP surgery, 11 revoked their consent before the operation, leaving 215 (97.7%) to take part in the baseline interview. The follow-up questionnaires were received from 193 (89.7%) patients at 3 months and 185 (86.0%) at 6 months after the operation. The primary reasons for leaving the follow-up schedule included having declined further participation (n = 8), lost to follow-up for unknown reasons (n = 8), relocation (n = 10), died for reasons unrelated to complication of prolapse treatment (n = 2), or incomplete data (n = 2). There was no difference in the symptoms (POP-SS and PHQ), body image, POP stage, or P-QoL scores between the patients who participated/did not participate in the follow-up (p > 0.05, Additional file 1: Table S1).
A large number had had POP for a long time before seeking treatment (median = 5.2; range 1–26 years). Reasons reported as the main barriers to seeking early treatment were lack of money (21.2%), fear of disclosure (15.9%), the perception that POP is incurable (13.6%), fear of treatment outcome (12.1%), lack of accompanying support (8.6%), distance from a health facility (requiring 2 days or more to reach health facility; 6.2%), and lack of transportation (5.0%). Three out of five patients (59.5%) had the decision making power to visit a health care facility when getting sick.
Patients’ characteristics are shown in Table 1. The mean age at the time of surgery was 49.3 ± 9.4 (range 35–70) years. Preoperatively, 148 (68.8%), 134 (62.3%), and 72 (33.5%) patients had anterior, central, and posterior descent ≥ III stages, respectively. These defects were associated with variable degrees of loss of support at the other vaginal sites considered, thus 131 patients (60.9%) showed descent in all three compartments, 50 (23.3%) in two compartments, and 34 (15.8%) in only one compartment (18 anterior descent and 16 apical descent).
Intraoperative and postoperative results were collected. The median operative time for all the surgical interventions was 65 (47–127) minutes, and the median postoperative hospital stay was 2 days (range, 2–4 days). No intraoperative complications such as severe haemorrhaging or rectal, bladder, or ureteric injuries occurred. However, some women developed mild to moderate postoperative complications: seven cases (3.2%) of fever and 11 (5.1%) of urinary tract infection. Late complications were also reported and included two cases (1.1%) of gluteal pain, four cases (2.5%) of dyspareunia, five cases (2.7%) of stress urinary incontinence, six cases (3.2%) of recurrent urinary tract infections, and five cases (2.7%) of constipation.
Effect of prolapse surgery on patient’s subjective outcomes
A significant improvement in quality of life was reported throughout the study (Fig. 1 and Table 2). In Fig. 1, the bar chart shows the figures (Mean ± SD) for P-QoL, POP-SS, BIPOP, and PHQ at 3 and 6 months after surgery compared to patients’ scores before surgery. The internal consistency (Cronbach’s alpha) of the P-QoL, POP-SS, BIPOP, and PHQ instrument in this study was 0.92, 0.75, 0.81, and 0.71, respectively.
Scores of patient-reported outcome instruments before and after surgical repair of prolapse (Mean ± SD). GHP general health perception, PI prolapse impact, RL role limitation, PL physical limitation, SL social limitation, PR personal relationships, EMO emotional disturbances, SE sleep/energy, SM severity measures, PC physical component, PSC psychological component, PRC personal relationship component, POP-SS pelvic organ prolapse symptom score, BIPOP body image in pelvic organ prolapse, PHQ patient health questionnaire, PRO patient-reported outcome
Prolapse quality of life
Preoperatively, the negative effects on personal relationships (76.7/100 points) and negative impact on physical impairment and roles (75.5 and 74.5/100 points) were those areas of patients’ HRQoL most affected. A significant improvement was reported after the 3 month follow-up for the above-listed domains. However, this improvement was not reproduced in the personal relationship domain score during this follow-up period, as the patient had a worse score (15.0 ± 12.6 to 20.0 ± 18.3, p = 0.005, paired t test). The 6-month follow-up demonstrated a further significant improvement as compared to the baseline. Similar improvement was also reported in the other P-QoL areas (GHP, SE, and SM) in both follow-ups (baseline vs. 6-month follow-up, out of 100 points in each case: 60.5 vs. 21.8; 46.7 vs. 14.4; 46.2 vs. 8.5; Additional file 1: Table S2).
P-QoL was also higher as measured by PRC, PC, and PSC at baseline. Nevertheless, a marked improvement was observed at a 6 month follow-up (mean change at baseline and 6 months with a 95% CI in each case: − 58.1 (− 61.8, − 54.4), − 49.4 (− 51.5, − 47.2) and − 40.1 (− 43.6, − 36.4), Table 2).
Prolapse symptoms score
A significant reduction in POP symptoms was detected (Table 2). The POP-SS score decreased at the 3 month follow-up, and the decrease was sustained at the 6-month follow-up (the mean decreased 5.2 and 2.1 points, respectively). At baseline, discomfort/pain that worsens when standing (85.1%), feeling something coming down (82.7%), and feeling heaviness around the lower abdomen (81.4%) were reported. These symptoms were reduced significantly after surgery. A total of 14.0% (n = 166) of patients reported a bothersome bulge symptom at 3 months after surgery, and 97.3% (n = 180) did not report this symptom at 6 months postoperatively (Additional file 1: Table S2).
Depressive symptoms
A total of PHQ-9 scores > 10 occurred in 42.8% (92/215) of the patients at baseline. After 6 months, the PHQ-9 scores significantly decreased. The mean change PHQ from baseline to 6 months was − 8.8 (95% CI: − 9.9, − 7.7 points, Table 2). The postoperative prevalence of depressive symptoms was 7.0% (13/185), which was six-fold lower compared to baseline. Items representing alterations in doing things, energy, and hope were the most commonly reported items at baseline (Additional file 1: Table S2).
Body image
Improvement in the BIPOP score was observed, indicating a better BI perception after surgery. Before surgery, 115 patients (53.8%) reported having regular sexual intercourse, while 18 (15.6%) had dyspareunia. Conversely, 6 months after surgery, 159 (85.9%) reported having regular sexual intercourse and 4 (2.5%) had dyspareunia (Additional file 1: Table S2). The BIPOP score (mean of 95%CI) was 33.9 (33.0, 35.2) versus 17.4 (16.6, 18.2) preoperative and at the 6 month follow-up, respectively (p < 0.001, Table 2).
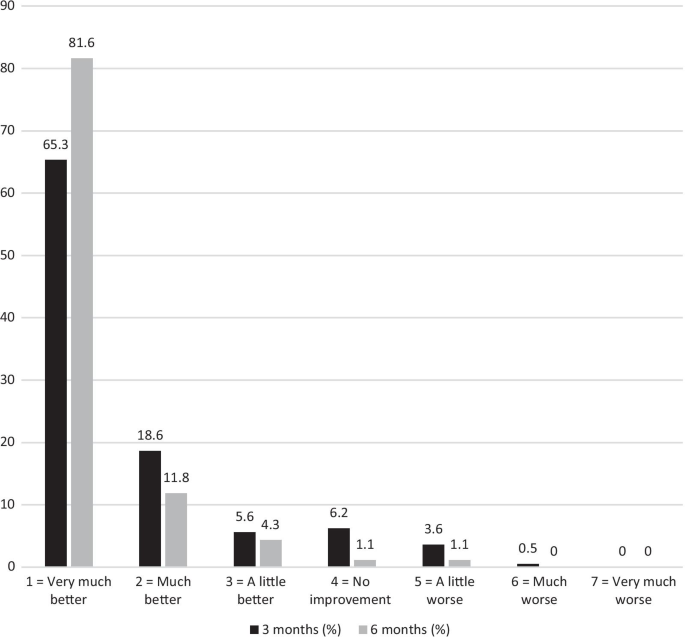
Patient global impression of improvement
Response to the surgical treatment measured by the PGI-I is shown in Fig. 2. Altogether, 97.8% of the patients considered their condition to be better, and 1.1% considered it to be worse compared to the preoperative situation at the 6-month follow-up (PGI-I scales 1–3, Fig. 2). At the 6-month follow-up, 171 (92.4%) patients recommended the operation to a close friend suffering from POP.
Goal attainment
Two hundred and ten women completed the preoperative goal assessment (97.6%). The most common patient goal was to reduce condition-specific symptoms, namely prolapse (186, 88.5%), urinary (174, 82.5%), and bowel symptoms (96, 45.7%), followed by improving intimate relationships (74, 35.2%), activities and social life (66, 31.4%), as well as body image/physical appearance (60, 28.5%) and general health (47, 22.3%). Living happily (74, 35.2%), reduced discomfort/pain (14, 6.7%) and other concerns (22, 10.5%) were also reported. One hundred sixty-six (89.7%) of 185 women achieved their goal of reducing prolapse symptoms (defined as score ≥ 6/10) at 6 month follow-up.
Predictors of quality of life change during follow-up
Linear Mixed Model (LMM) analysis was performed to examine the longitudinal effects of sociodemographics, POP-SS, BIPOP, and PHQ on P-QoL domains and/or components (Table 3). The change in P-QoL after surgery was associated with the change in POP-SS, PHQ, and BIPOP scores (p < 0.001). There was a change in PC and PRC scores overtime for a point change in the POP-SS, PHQ, and BIPOP scores (p < 0.001). Being married resulted in a 5.7 point increase in the PRC score (p < 0.01). However, age, parity, type of surgery, and prolapse stage were not associated with the improvement of P-QoL scores (Table 3).